Why Obstructive Sleep Apnea Increases Cardiovascular Risk

When a patient joins my practice, I always ask about sleep.
I do this for three reasons:
-
There is a relationship between short sleep and worse cardiovascular outcomes.
-
Poor sleep generally impacts cognitive well-being, nutrition and exercise routines, all of which are key pillars of cardiovascular health.
-
To assess if they have a sleep condition called obstructive sleep apnea, which is also tightly linked to cardiovascular disease and can be treated.
I have spoken in depth about the first two items on this list previously.
Today, I want to focus on the medical condition of obstructive sleep apnea (OSA) and why it matters for cardiovascular health.
Now, before you check out and say, this doesn't apply to me, just know that the majority of sleep apnea is undiagnosed1.
Approximately 90% of those identified as being at high risk for OSA on population surveys had no prior identification of sleep apnea.
So don’t be so quick to think this issue doesn’t apply to you.
About one-third of middle-aged males and nearly one in five middle-aged females have obstructive sleep apnea.
It is common and frequently goes undetected, which is a very bad thing.
What Is Obstructive Sleep Apnea?
During sleep, your airways should remain open so you can breathe.
Seems pretty reasonable, right?
Not so for those with OSA.
For people with OSA during sleep, there are recurrent episodes where the airway collapses and obstructs the passage of air to the lungs, resulting in:
-
Lack of oxygen
-
Significant variations in blood pressure, heart rate and other physiological metrics.
-
Broken sleep (That you are likely unaware of)
That is the somewhat technical definition of obstructive sleep apnea, but a sleep physician colleague explained it to me slightly differently to make a point.
“Imagine when you are asleep, someone comes into your room, puts their hands around your throat to the point where you can no longer breathe and starves your body of oxygen.
You desperately want to breathe, so you choke and gag in response, and your heart rate and blood pressure go through the roof.
You usually have no idea this is happening and often have limited recollection of it in the morning.
Now imagine someone doing that to you every night.
Repeatedly.
Sometimes 30 times per hour.
And when it happens less than 15 times an hour, we call it ‘mild’.
That is what obstructive sleep apnea is.”
I quickly got the point.
Not good.
What are the cardiovascular consequences?
As described above, in middle-aged adults, it impacts between 17 and 34% of the population.
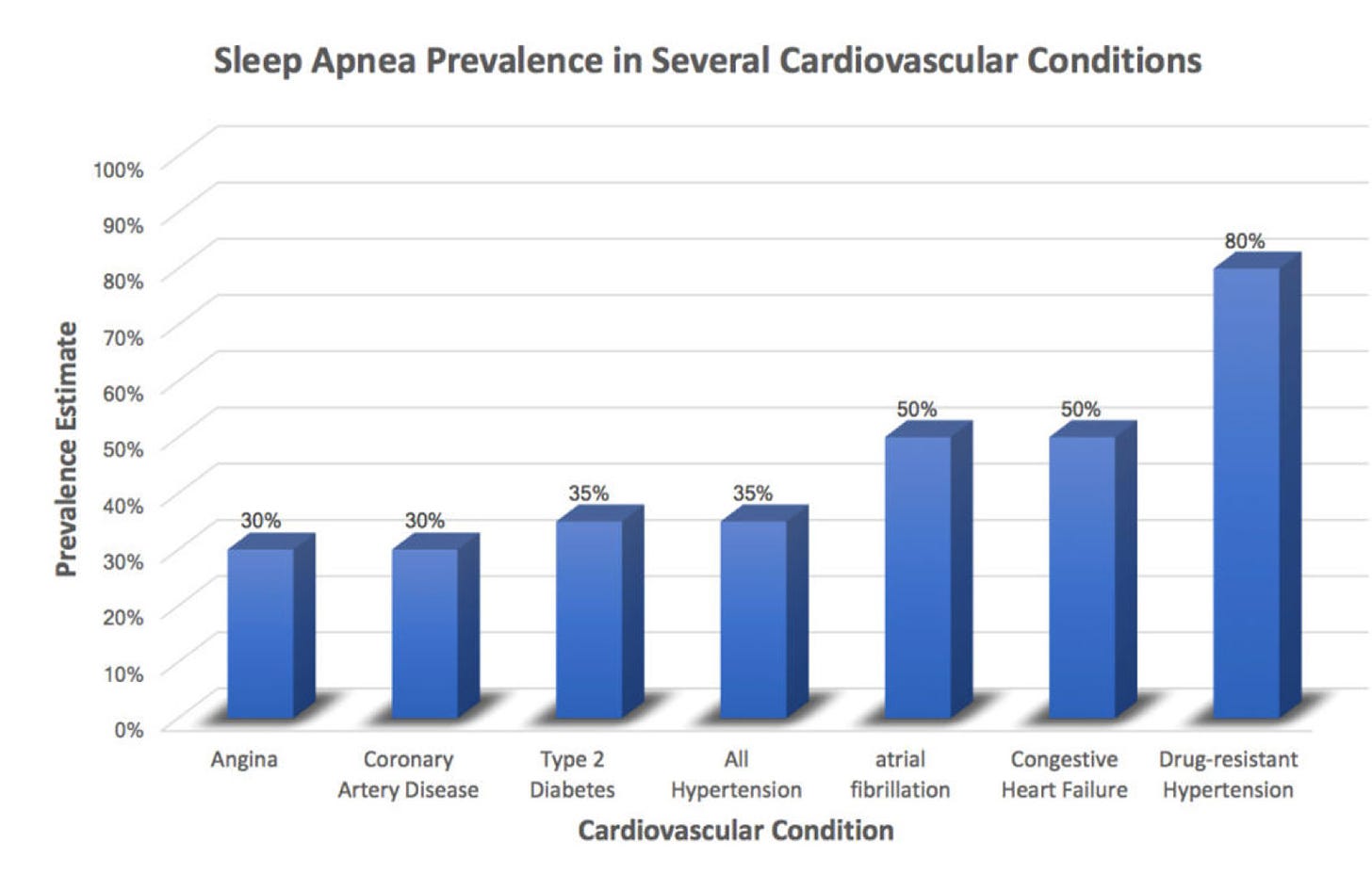
However, it's quite a different story for people with high blood pressure and other cardiovascular conditions.
40 to 80% of those with high blood pressure, heart failure, coronary artery disease, atrial fibrillation and stroke have OSA.
If you have high blood pressure or atrial fibrillation, there is a very high chance that you could also have OSA.
If you have resistant high blood pressure, i.e. you need multiple medications to control your blood pressure, there is about an 80% chance you have OSA2.
People with OSA have much higher rates of cardiovascular disease as measured by levels of coronary artery calcification and, in general, are about twice as likely to have a cardiovascular event or die from cardiovascular disease3.
There is also a very strong relationship with stroke and stroke recurrence.
Why Does OSA Increase Cardiovascular Risk?
The reasons why OSA increase the risk of cardiovascular disease are not entirely clear.
The main reasons are thought to relate to:
-
Large fluctuations in blood pressure
-
Subsequent damage to the lining of the artery wall
-
Oxidative stress
-
Systemic inflammation
-
Excess clotting

How Do You Know If You Have OSA?
The diagnosis of obstructive sleep apnea is made during a sleep study using continuous assessment of your breathing, oxygen levels, chest movement, etc.
This is usually done in a sleep lab but can increasingly be done in the home environment.
However, you can answer a few short questions to give you a good indication if OSA might be an issue for you.
The STOP-BANG Questionnaire:
-
Do you SNORE loudly (louder than talking or loud
enough to be heard through closed doors)?
-
Do you often feel TIRED, fatigued, or sleepy during daytime?
-
Has anyone OBSERVED you stop breathing during your sleep?
-
Do you have or are you being treated for high blood PRESSURE?
-
BMI more than 35kg/m2?
-
AGE over 50 years old?
-
NECK circumference > 16 inches (40cm)?
-
Male?
If you answered ‘Yes’ to five or more of these items, you are at a high risk of having obstructive sleep apnea and consultation with a sleep physician is likely warranted.
How is it treated?
Because there is such a close relationship with obesity, the first line of treatment is usually weight loss.
Even a 10% weight loss can substantially reduce the number of apnea episodes a patient experiences, their need for mechanical breathing supports and also improve daytime symptoms of fatigue4.
For patients with moderate to severe OSA, assisted breathing support is usually required using CPAP (Continuous Positive Airway Pressure) therapy.
For mild cases, mouth-worn devices can be of value.
However, please go back to my colleagues’ original description of ‘mild OSA’, which involves someone choking you only 14 times or less per hour when you sleep.
Mild is an understatement.
Metabolic Syndrome
There is no doubt that metabolic dysfunction is closely linked to OSA.
60% of patients with OSA have metabolic syndrome5.
Metabolic syndrome is largely preventable, suggesting that OSA could also be preventable.
Metabolic syndrome is also eminently reversible with appropriate lifestyle changes, suggesting that many of the adverse cardiovascular effects of OSA could be reversible also.
At the base of these two conditions is insulin resistance.
This is not to say that insulin resistance causes OSA, but avoiding it certainly decreases the likelihood of developing OSA.
Takeaway
Obstructive sleep apnea is common.
It frequently goes undiagnosed.
It significantly increases the risk of heart attack, stroke and atrial fibrillation.
It is potentially avoidable.
So, if you are the person that no one will share a hotel room with because of your snoring?
Then, it might be time to fill out the rest of the STOP BANG questionnaire.
Because your poor sleep might be more than just a nuisance.
Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021 Jul 20;144(3):e56-e67.
Cardiovascular Disease Risk in Obstructive Sleep apnea: An Update. J Sleep Disord Ther. 2017;7(1):283.
Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021 Jul 20;144(3):e56-e67.
Dose-response relationship between weight loss and improvements in obstructive sleep apnea severity after a diet/lifestyle intervention: secondary analyses of the “MIMOSA” randomized clinical trial. J Clin Sleep Med. 2022;18(5):1251–1261.
Relationship of metabolic syndrome and obstructive sleep apnea. J Clin Sleep Med. 2007 Aug 15;3(5):467-72.




